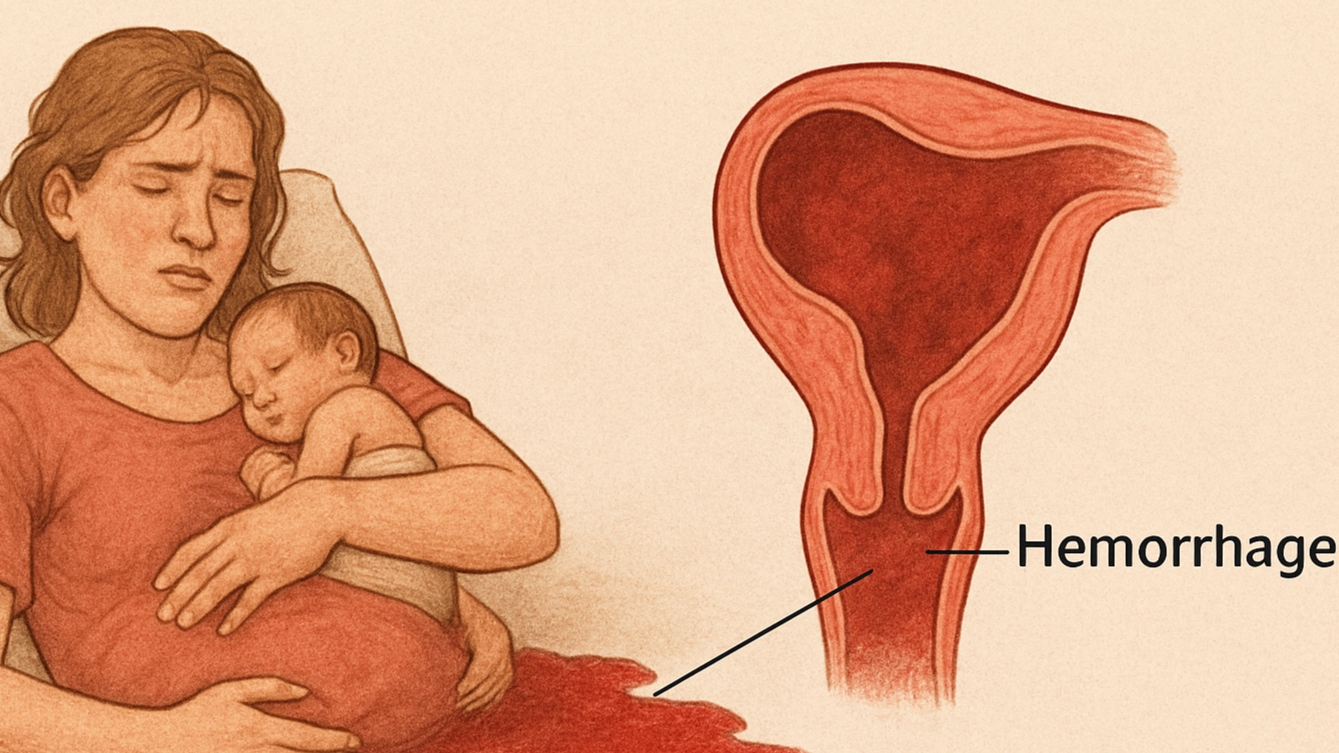
Postpartum Hemorrhage
Postpartum Hemorrhage: A Silent Threat After Childbirth
Childbirth should be a moment of joy, but for many women, it can turn life-threatening in a matter of minutes. One of the leading causes of maternal death worldwide is Postpartum Hemorrhage (PPH)—a dangerous complication that demands urgent attention, awareness, and action. Understanding this condition can help save lives—because with the right knowledge and response, PPH is both preventable and treatable.
What is Postpartum Hemorrhage?
Postpartum Hemorrhage refers to excessive bleeding after childbirth, typically defined as the loss of more than 500 ml of blood after vaginal delivery or more than 1,000 ml after a cesarean section. PPH can occur within the first 24 hours (primary PPH) or between 24 hours and 6 weeks after delivery (secondary PPH). It is a medical emergency that can rapidly lead to shock, organ failure, or death if not managed quickly and effectively.
What Causes Postpartum Hemorrhage?
PPH can be caused by several factors, often remembered using the “4 Ts”:
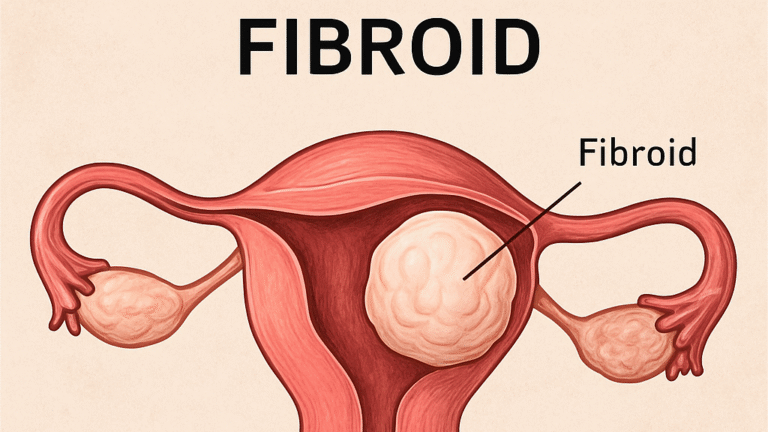
1. Tone – Uterine atony (the uterus fails to contract after delivery), the most common cause
2. Tissue – Retained placental fragments that prevent proper uterine contraction.
3. Trauma – Tears or lacerations in the cervix, vagina, or uterus.
4. Thrombin – Blood clotting disorders that affect the body’s ability to stop bleeding.
Other risk factors include prolonged labor, multiple births, large babies, overuse of labor-inducing drugs, previous PPH history, and cesarean delivery.
Symptoms of Postpartum Hemorrhage
The signs of PPH can develop suddenly and worsen rapidly. Key symptoms include:
Uncontrolled bleeding from the vagina
Drop in blood pressure
Increased heart rate or palpitations
Pale or cold skin
Dizziness or fainting
Swelling or pain in the vagina or perineum (in cases of internal bleeding)
Immediate medical attention is critical. Delays can lead to severe complications, including death.
How to Prevent Postpartum Hemorrhage
While not all cases are preventable, most can be anticipated and managed with good maternal care. Key prevention strategies include:
Active management of the third stage of labor (AMTSL), which includes giving uterotonic drugs like oxytocin immediately after delivery.
Proper training of birth attendants to recognize early warning signs.
Routine monitoring of vital signs and bleeding after birth.
Regular prenatal care to identify and manage risk factors.
Ensuring delivery occurs in a well-equipped facility with skilled personnel and emergency supplies.
Community education also plays a role—mothers and families should know when to seek urgent care.
Best Treatment for Postpartum Hemorrhage
PPH treatment is time-sensitive and involves a combination of medical and surgical interventions depending on severity:
Medications: Uterotonics like oxytocin, misoprostol, or ergometrine to stimulate uterine contractions.
Manual removal of retained placenta or clots.
Blood transfusions to replace lost blood.
IV fluids and oxygen to stabilize the mother.
Surgical options such as uterine artery ligation, balloon tamponade, or hysterectomy in extreme cases.
Tranexamic acid may be used to reduce bleeding.
Summary
Postpartum Hemorrhage (PPH) is a serious and potentially life-threatening complication that involves excessive bleeding after childbirth, typically more than 500 ml after vaginal delivery or over 1,000 ml after a cesarean section. It can occur within 24 hours or up to six weeks after delivery. The main causes include uterine atony (failure of the uterus to contract), retained placental tissue, trauma during delivery, and blood clotting disorders. Symptoms include heavy bleeding, low blood pressure, rapid heartbeat, dizziness, and pale or cold skin. While not all cases are preventable, most can be managed through skilled maternal care, early recognition, and preventive measures such as administering uterotonic drugs immediately after birth. Treatment requires rapid response and may involve medications, blood transfusions, manual procedures, or surgery depending on severity. With proper prenatal care and timely intervention, PPH can be effectively managed, and many maternal deaths can be prevented.